Menstrual pain
Menstrual pain is neither rare nor trivial. Whether young girl or seasoned woman: Almost every woman has had period pain - and millions suffer from it month after month.

Contents:
From a medical point of view, there is usually no reason to concern - some women even simply accept menstrual pain as anunchangeable side effect of fertility. For most people, however, period pain is an unacceptable “inconvenience” in their daily lives.
And rightly so, because the dull or cramping abdominal pain, which often radiates to the back or thighs, interferes with almost all everyday activities. Often, they even lead to school absences or inability to work, or at least to a reduction in quality of life and mobility: A current representative online survey on the topic of menstrual pains among more than 1,000 women between 14 and 45 years of age showed that 81 percent suffer from pain during their menstruation - and 88 percent of them would like to actively do something about it.
How does menstrual pain arise and what are its causes?
The typical symptom of painful menstruation is lower abdominal pain. The pain is cramp-like or appears as a dull continuous pain, most severe in the first 24 hours of menstruation. Good to know: Most of the time, abdominal pain during the menstruation is not an illness, but has completely natural causes - the turbulent interplay of female hormones. They control the menstrual cycle, which lasts for an average of 28 days and is - right after the natural sleep rhythm - the most important clock in a woman’s life. In some cases, however, extremely severe menstrual pain can indicate endometriosis (a growth of the lining of the uterus), a myoma (a benign growth of the uterine muscles) or a cyst (a fluid-filled cavity, such as in the ovaries). If an illness is suspected, a gynaecological evaluation should be carried out.
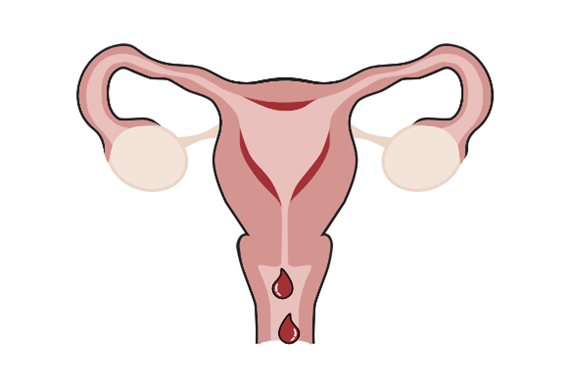
What exactly are the causes of abdominal cramps? In the first two weeks of the cycle, hormones stimulate the production of eggs and ensure that ovulation occurs in the middle of the cycle. After menstruation, the preparation for a possible pregnancy starts and the uterus builds up a thick, well perfused mucous membrane again.
Shortly before ovulation, the oestrogen level rises rapidly: During these days, women have a greater sexual desire. With ovulation, which usually takes place around the 14th day of the cycle, the oestrogen content of the blood drops again. Now progesterone, which is responsible for the remodelling of the uterine lining, takes over. However, if fertilisation does not occur in the following days, the lining of the uterus is broken down, the uterus contractions and a feeling of tension in the chest occurs. Women can suffer from mood swings and in addition, water retention and digestive problems can occur, for example. Such symptoms are typical of the so-called premenstrual syndrome, or PMS for short.
After about 28 days (depending on the menstrual cycle), menstruation begins and the remnants of the uterine lining are shed with the menstrual period - often accompanied by feelings of tension as well as pain and cramps in the lower abdomen. The reason for this are contractions triggered by hormones (prostaglandins). The contraction of the uterus impairs the blood flow, especially smaller vessels are essentially squeezed - which increases the pain and promotes the occurrence of other symptoms. And then the stressful pain is there.
Menstrual pain is the most common gynaecological complaint in women. If menstruation is regularly accompanied by persistent, cramping pain, medical experts speak of dysmenorrhoea. They distinguish between primary and secondary “acquired” dysmenorrhoea - although the symptoms of both forms are the same. Anyone who regularly suffers from menstrual cramps and abdominal cramps should therefore generally talk to a health professional to rule out pathological triggers.
Primary or secondary menstrual pain?
Primary period pain often occurs from the first menstrual period onwards - but only becomes fully pronounced when the body has adjusted to the menstrual cycle. Other forms of joint pain are more likely to need heat treatments. This is due to an overproduction of certain hormones, so-called “uterine prostaglandins”. These stimulate the uterine muscles so that the mucous membrane can be rejected. The contraction of the uterus impairs the blood flow, especially smaller vessels are essentially squeezed - which increases the pain and promotes the occurrence of other symptoms. Unfortunately, there is no cure-all for menstrual pain yet. Nevertheless, women do not have to helplessly accept these unpleasant accompanying symptoms of their menstruation, but can do a lot against them with simple means - for example, with relaxation exercises, in part also by taking the contraceptive pill, and last but not least, with heat applications.
Secondary menstrual pain is far less common. They have an organic cause and therefore usually only appear in middle age. The underlying condition must be determined and treated here. Secondary menstrual pain can be caused by endometriosis (an overgrowth of the uterine lining), a myoma (a benign growth of the uterine muscles) or cysts (cavities filled with fluid, for example in the ovaries). In addition, the use of mechanical contraceptives such as the IUD can sometimes lead to secondary menstrual pain.
Symptoms of menstrual pain
Menstrual complaints? Every woman experiences it a little differently, with impairments ranging from mild discomfort to significant cramping. However, most women are familiar with menstrual pain, i.e. pain in the lower abdomen during their period.
Period pain has many faces, it can include pulling and cramps or present themselves as a dull continuous pain, usually strongest in the first 24 hours of bleeding. It is not uncommon for pain to radiate into the back or thighs, and sometimes it takes on violent proportions. Although recurring menstrual pain is not caused by illness in most of the cases, the underlying hormones work throughout the body. This is why period pain is often accompanied by other symptoms.
These include among others:
· General indisposition
· Circulation problems
· Nausea up to and including vomiting
· Diarrhoea
· Headaches
· Irritability and mood swings
· Weight increase

Quite a few women are so severely affected that they cannot go to school or work. Fortunately, however, the symptoms of menstruation usually subside after one to two days. In addition, lifestyle changes and simple home remedies can significantly help to alleviate them.
Risk factors
Why do I have such pain and other women don’t? This is a question asked by many who suffer from monthly period pains for which no medical cause has been found.
But the answer is not always easy. This is because there are numerous factors that favour the occurrence of abdominal pain and other symptoms. The most important ones are:
-
Age: Young and childless women suffer more often from menstrual pain. After childbirth and with age, the symptoms usually become less severe.
-
Early menstruation: Those who experience their first menstrual period (menarche) at the age of twelve or earlier are more at risk.
-
Diets: Trying to reduce body weight can also increase the pain. Similarly, very slim women - with a body mass index below 20 - often have more severe symptoms.
-
Cycle intensity and length: Women with heavy, prolonged or irregular periods often develop more severe pain.
-
Lifestyle: Smoking clearly has a negative influence on the severity of period pain. Whether these are also influenced by alcohol and lack of exercise has not yet been fully clarified. On the other hand, the negative influences of stress can be clearly identified - those who are under psychological pressure often literally feel more pressure in their abdomen.
-
Uterine abnormalities: If the uterus is very small or not quite properly positioned in the abdomen, this can also make its contractions painful.
-

THERMACARE® For menstrual pain
for the treatment of menstrual pain
What helps for menstrual pain
Unfortunately, menstrual pain cannot be totally managed - and there is no generally effective therapy. Some women take pain-relieving or antispasmodic medication for their symptoms, others swear by relaxation techniques such as yoga or autogenic training. Even if they do not have a pathological cause in most women: Menstrual pain and its accompanying symptoms are no trivial matter. After all, they cause distress and considerably restrict the active everyday life of affected women.
In addition, menstrual pain sometimes leads to social and/or psychological conflicts, for example because you cannot appear at work or simply no longer feel comfortable in your own body and also suffer mentally from the pain and other symptoms of the menstruation. Therefore, no woman should simply give up with menstrual pain - but actively do something about it. Here we have listed some of the most important treatment methods for you and show you which therapy helps quickly and effectively.
- Drug treatment for menstrual pain
-
The drug therapy of menstrual pain is mostly done with painkillers available without a prescription, especially so-called non-steroidal anti-inflammatory drugs (NSAIDs) with the active ingredients Naproxen and Ibuprofen or Paracetamol. The advantage: Among other things, these substances ensure that less prostaglandin is produced. This reduces the discomfort, as this hormone is responsible for the excessively strong contractions of the uterus and thus also for the poorer blood flow to the organ. However, due to their side effects, such painkillers should not be taken too often or for longer than four days at a time without a doctor’s instructions.
Active substances such as the antispasmodic butylscopolamine are also often helpful for abdominal pain - especially if it is labour-like or even colicky. In addition, the use of hormonal contraceptives such as the contraceptive pill or a hormonal IUD improves menstrual symptoms considerably in many people. Naturally, this option is only suitable for women who do not currently wish to have children or who do not have any health restrictions that would prevent them from doing so.
- Non-drug treatment for menstrual pain
-
Since many women do not want to burden their bodies with chemicals on a regular basis, they resort to non-drug remedies to quickly get their period pain under control. Here, the hot favourite has always been heat - whether in the form of a hot bath, a hot water bottle or a visit to the sauna. Unfortunately, the relaxing and pain-relieving effect wears off relatively quickly - and while you are using it, you are also locally bound and only able to use it to a limited extent during the critical days. Modern women cannot and do not want to accept that. They ask themselves: “Isn’t there anything other than painkillers or lying on the sofa with a hot water bottle? How can I continue to participate in everyday life? What else helps against period pain?” ThermaCare® for menstrual pain is the solution, thanks to the therapeutic heat released by its cells technology
An improved deep heat therapy tailored to the needs of active women, that can be used for long-lasting, mobile and discreet relief - that is what the self-heating ThermaCare® HeatWraps for menstrual pain offer: Due to a controlled oxidation process, they unfold soothing heat of a constant approx. 40 °C that lasts for eight hours. In contrast to hot water bottles and the like, the muscles are relaxed, constricted blood vessels are permanently widened and the blood circulation is stimulated. This improves the oxygen supply in the abdomen. The result: Tension and cramp is released. Period pains are relieved naturally. In a controlled scientific study, this deep heat was found by sufferers to be just as effective as ibuprofen1. There was also a significant improvement in certain quality of life values (such as cramps and tenderness in the chest)1 during menstruation in primary dysmenorrhea compared to the non-warming wrap. ThermaCare® HeatWraps for menstrual pain are simply stuck into the panties, leggings / tights or the vest: There they hold reliably, go along with every movement and thus enable more relaxed days.
1 Akin, M. D., et al. (2001). “Continuous low-level topical heat in the treatment of dysmenorrhea.”
- More tips for menstrual pain
-
In addition to the application of heat, there is a lot more you can do about hormone-related complaints such as abdominal cramps during the menstruation. These include healing teas, conscious relaxation and meditation, massages, exercise and a balanced diet.
- Exercise for menstrual pain relief
-
Exercise is a very simple way to relieve menstrual pain. Even a little walking or cycling, a walk in the fresh air or light gymnastics (for example, from the repertoire of pelvic floor gymnastics) have an important role in relaxing muscles that are tense during the days and improving the blood circulation in the pelvic area as well as in the lower abdomen. Some analyses also suggest that regular exercise even prevents annoying period pain - regardless of the type of sport. If you want to specifically relax the pelvic region, you should attend a course for targeted pelvic floor training or buy a corresponding manual from a bookstore.
- Tea for menstrual cramp relief
-
Healing teas with antispasmodic goose fingerweed, yarrow or lady’s mantle or with relaxing herbs such as lemon balm and chamomile have also proven effective for abdominal pain. Teas with St. John’s wort can help to overcome accompanying low moods. Rosemary tea helps with circulatory problems. However, when using tea, it should be noted that some types of tea can interact with the pill. For example, taking St. John’s wort can impair the effect of hormonal contraceptives such as the pill or hormone patches, or lead to increased bleeding between periods.
- Diet for menstrual pain
-
It is well known that a balanced diet has a positive influence on health and well-being. However, what many do not know: It can also reduce menstrual pain and abdominal cramps. Medical experts advise affected women to eat a high-fibre diet with plenty of fruit and vegetables and whole grain products. Especially in the second half of the cycle and during the menstruation itself, it can also be worthwhile to reduce the salt intake. Because salt promotes water retention. To ensure that enough blood-forming iron is available, eating meat during menstruation is recommended.
However, it is better to stay away from products that contain a lot of arachidonic acid, such as pork liver and lard and egg yolks. This is because prostaglandins, i.e. hormones that promote menstrual pain, can be formed from this acid. We recommend eating nuts, wheat germ and whole grain rice. Because these foods contain a lot of magnesium, which can prevent muscle cramps.
- Relaxation for menstrual pain relief
-
Whether autogenic training, yoga, qigong or other techniques of meditation and relaxation: Taking pressure off the psyche also relieves the strained uterus.
Aromatherapy, for example, is also helpful because essential oils stimulate our limbic system, the part of the brain that is responsible for our emotions. That is why fragrances have always been used to promote our emotional balance.
A few examples
· Lavender scent soothes
· Jasmin is optimistic
· Rosemary vitalises and cheers up
· Vanilla soothes, comforts and curbs hunger for sweets
· Rose soothes anxieties
· Lemon and grapefruit cheer up and have an invigorating effect
· Peppermint oil helps with headaches
You can simply sniff a bottle with the corresponding essential oil or put a few drops of it into the water of a fragrance lamp. The beneficial effect already sets in. Alternatively, you can buy a massage oil with the right fragrance. A few drops of it are then simply massaged in clockwise around the navel with gentle movements.The following breathing technique, in which you can simply let out some air, is a playful way to relax. Because when we are under pressure, we usually inhale excessively - and become nervous. In such moments, one should pull the “breathing brake”: First inhale deeply through your nose. On the subsequent exhalation, press the lips together and blow out the air against the resistance with a very fine jet of air. Repeat five times. It calms you down in no time.
FREQUENTLY ASKED QUESTIONS
- What helps relieve menstrual pain?
-
Painkillers such as Ibuprofen or Paracetamol help with menstrual pain. A comparably strong but natural pain relief can be achieved by heat, for example by ThermaCare® HeatWraps. Also helpful are antispasmodic teas, relaxation, light exercise and aromatherapy.
- What home remedies help with period pain?
-
Tried and tested home remedies for menstrual pain are the application of heat (e.g. ThermaCare® HeatWraps, hot water bottle, warm bath or heated cherry stone pillow) and antispasmodic and relaxing teas that contain fingerweed, yarrow or lady’s mantle.
- Why do women have abdominal pain during menstruation?
-
In the first half of the cycle, a thick mucous membrane with a good blood supply is built up in the uterus. If fertilisation does not occur in the middle of the cycle (around day 14, depending on the cycle), it is broken down again. The reason for the pain is contractions triggered by hormones (prostaglandins). The contraction of the uterus impairs the blood flow, especially smaller vessels are essentially squeezed - which increases the pain and promotes the occurrence of other symptoms.
- Which pill/tablet or medicine helps relieve menstrual pain?
-
Painkillers available without a prescription, especially so-called nonsteroidal anti-inflammatory drugs (NSAIDs) with the active ingredients Naproxen or Ibuprofen, the analgesic Paracetamol and active ingredients such as the antispasmodic butylscopolamine are suitable for the medicinal therapy of menstrual symptoms and abdominal pain, if these medicines are tolerated.
The use of hormonal contraceptives such as birth control pills or a hormone coil also have a strong pain-reducing effect for many sufferers. However, these should only be used if there is no desire to have children or if there are no health reasons for not doing so. - Which tea helps with menstrual pain?
-
The teas for abdominal pain include herbal teas with antispasmodic goose fingerweed or relaxing herbs such as lemon balm and chamomile. St. John’s wort tea can be supportive in the case of accompanying depressed moods. Rosemary tea helps against circulatory problems. However, when using tea, it should be noted that some types of tea can interact with the pill. For example, taking St. John’s wort can impair the effect of hormonal contraceptives such as the pill or hormone patches, or lead to increased bleeding between periods.
- When do menstrual pains occur?
-
This depends on the individual cycle of the woman. Some women experience premenstrual syndrome (PMS) as painful, for others the pain only starts with the first day of their period. Most women complain of the most severe pain in the first 24 hours of menstruation.